Medical negligence and the Bolam test
How is medical negligence determined?

Negligence exam scenarios may involve a defendant who is a medical practitioner such as a doctor, nurse, paramedic or dentist. Students are typically expected to explain and apply the elements of duty, breach and damage. There is usually little difficulty in establishing that a medical practitioner owes a duty of care to a patient, e.g. using an earlier precedent such as Wilsher v Essex AHA (1988). The issue of whether the duty has been breached will be less clear and will be central to the success of any claim involving a medical practitioner.
In the past it has proven difficult to determine the standard of acceptable medical practice because if the standard is set too low it is likely to give rise to more medical negligence claims, as more claimants will be able to prove breach. However, if the standard is set too high, this would be a barrier to a claim for medical negligence and could therefore result in injustice.
The Bolam test
It was held in Bolam v Friern Hospital Management Committee (1957) that a ‘doctor is not guilty of negligence if he has acted in accordance with a practice accepted as proper by a responsible body of medical men skilled in that particular art’.
In other words, if the medical practitioner has acted in a way that is different from the usual standard of care (as accepted by other practitioners in their profession) then they will have breached their duty. This is known as the Bolam test.
John Bolam suffered from depression. He was advised by the consultants treating him that he should have electroconvulsive therapy (ECT). This is a treatment that involves a brief electrical stimulation of the brain. Prior to this procedure he was not warned of any risks that could result from the ECT, nor offered any relaxant drugs by the medical team. During the procedure he ‘flailed about violently’ and consequently suffered a fractured hip. Bolam claimed that the doctors treating him should have alerted him to the risks and, failing to do so, breached their duty to him as a patient. This test can be criticised as medical practitioners, rather than judges, determine whether there has been a breach.
The Bolam test arguably creates a high threshold for the patient to prove as the ‘body of medical men’ that the courts are looking at does not need to be a substantial body but only a ‘minority’. In addition, the courts have acknowledged that reasonable medical professionals will differ in their views, and a medical practitioner will not be in breach of their duty just because ‘there is a body of opinion that would take a contrary view’.
In practical terms, this then means that it would be necessary for the claimant to prove that there is no body of medical opinion that would have approved of the way the medical practitioner acted in the circumstances to prove breach.
A key point to note is that it is not necessary for the body of medical opinion to agree that the medical practitioner had acted in an ideal way, just that their actions were in accordance with minimum accepted practice.
Although the Bolam test sets a low threshold for medical practitioners, this has been justified as judges are not medically trained and so are not in a position to ‘weigh up competing bodies of professional opinion’. However, in Bolitho v City and Hackney Health Authority (1996) it was determined that the judge must be satisfied that the body of opinion had a ‘logical basis’ that raised the threshold.
Patrick Bolitho
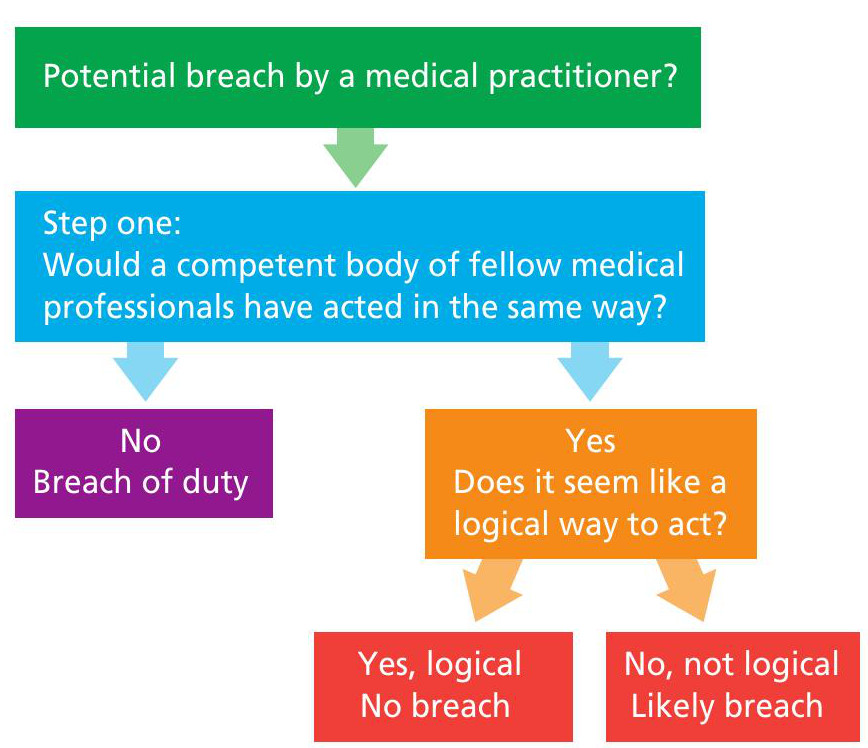
This is a variant on the Bolam test and it is arguably more robust. It is a two-stage test that works as follows:
1 Did the defendant act in accordance with the reasonably competent body of fellow professionals?
2 If so, is the expert opinion capable or not of ‘withstanding logical analysis’?
Two-year-old Patrick Bolitho was admitted to hospital with breathing difficulties. He suffered two episodes of respirator y failure while in hospital, and as a result he then suffered cardiac arrest that led to brain damage and consequently to his death.
There was a dispute about whether the treatment given to Bolitho was appropriate and his parents brought a claim in negligence against the health authority.
The court had to determine whether a competent doctor would have acted in the same way as the registrar who was responsible for Bolitho. Out of eight medical experts, five said that they would have acted in a different way and three stated they would have done the same as the registrar in this case.
The judge ruled that both groups could be regarded as a ‘responsible body of professional opinion’ and therefore the treatment given to Bolitho was not a breach of duty as it met the proper level of skill and competence even though other doctors would have acted differently.
The Court of Appeal upheld this decision but confirmed that if the opinion of a medical expert is illogical, then the court may determine that it is unreasonable (and so would result in the defendant breaching their duty).
‘If, in a rare case, it can be demonstrated that the professional opinion is not capable of withstanding logical analysis, the judge is entitled to hold that the body of opinion is not reasonable or responsible.’ (Lord Browne-Wilkinson)
In other words, if the expert opinion appears to be illogical then it could be determined that the medical practitioner was in breach of their duty, even if they have acted in accordance with the expert opinion.
Although Bolitho added an additional layer to the Bolam test and the added judicial control has been exercised in several cases, it has arguably not had a ‘dramatic impact on the law’ as it is rare for a judge to regard a medical expert’s view as unreasonable. How should students use the case of Bolitho in answering an exam question? Mention of the additional element from Bolitho is most relevant to the AO1 element (explanation of the law), as it is unlikely that the expert opinion of a body of medical professionals will be illogical and will require discussion in the application aspect (AO2 element) of an answer.
Informed consent
When considering breach of duty in relation to medical practitioners, it may be relevant for students to consider the issue of informed consent. This is because a failure to disclose the material risks of treatment or medical procedures and give the claimant an opportunity to consent is likely to amount to a breach of duty.
In Montgomery v Lanarkshire Health Board (2015) it was ruled that, in recognition of the fact that patients were autonomous individuals, doctors had an obligation to disclose any risk to which ‘a reasonable person in the patient’s position would attach significance’. The patient should therefore be told what they want to know, and not what the doctor thinks they should be told.
Nadine Montgomery gave birth to a son who suffered lifelong disabilities. She had previously asked her obstetrician whether a natural birth was appropriate and safe given that she was a woman of small stature, and the size of her unborn child. Although the doctor was aware of the risk of complications, she failed to communicate these to Montgomer y.
Evidence indicated that had the baby been delivered via caesarean section, he would have been born without injur y. Montgomery claimed that if she had known of the increased risk, she would have requested a caesarean section. The Supreme Court held that the obstetrician had breached her duty in failing to inform Montgomery of the risks.
As a result of the Montgomery case, medical practitioners have a duty to ensure that the patient is aware of any material risks involved with the recommended treatment. However, they can withhold information if they believe that it will be detrimental to the patient’s health.
In an exam question, students only need to refer to Montgomery if a scenario involves a patient consenting to treatment. If this is the case, students would need to discuss whether the reasonable person would want to know about the risks involved (would they attach significance to the risk). If so, the medical practitioner is obliged to inform them about those risks and failure to do so is likely to amount to a breach of their duty.





